Heart Disease in Women: The Silent Killer
Heart disease in women remains the leading cause of death in the United States, yet it’s often misunderstood, misdiagnosed, or ignored. Unlike the “classic” chest pain symptoms seen in men, women may experience subtle, atypical signs that are easy to overlook. Understanding these symptoms is key to early detection and saving lives. This article reveals the unique ways heart disease affects women and how to respond effectively.
Why Heart Disease in Women Often Goes Unnoticed
Many women—and even healthcare providers—fail to associate their symptoms with heart disease. Contributing factors include:
- Misinterpreted symptoms — Symptoms like fatigue or indigestion are often attributed to stress, aging, or menopause.
- Gender bias in medical research — Historically, most studies focused on men, delaying awareness of how heart disease presents in women.
- Lack of awareness — Many women don’t realize they’re at risk, especially if they lead relatively healthy lifestyles.
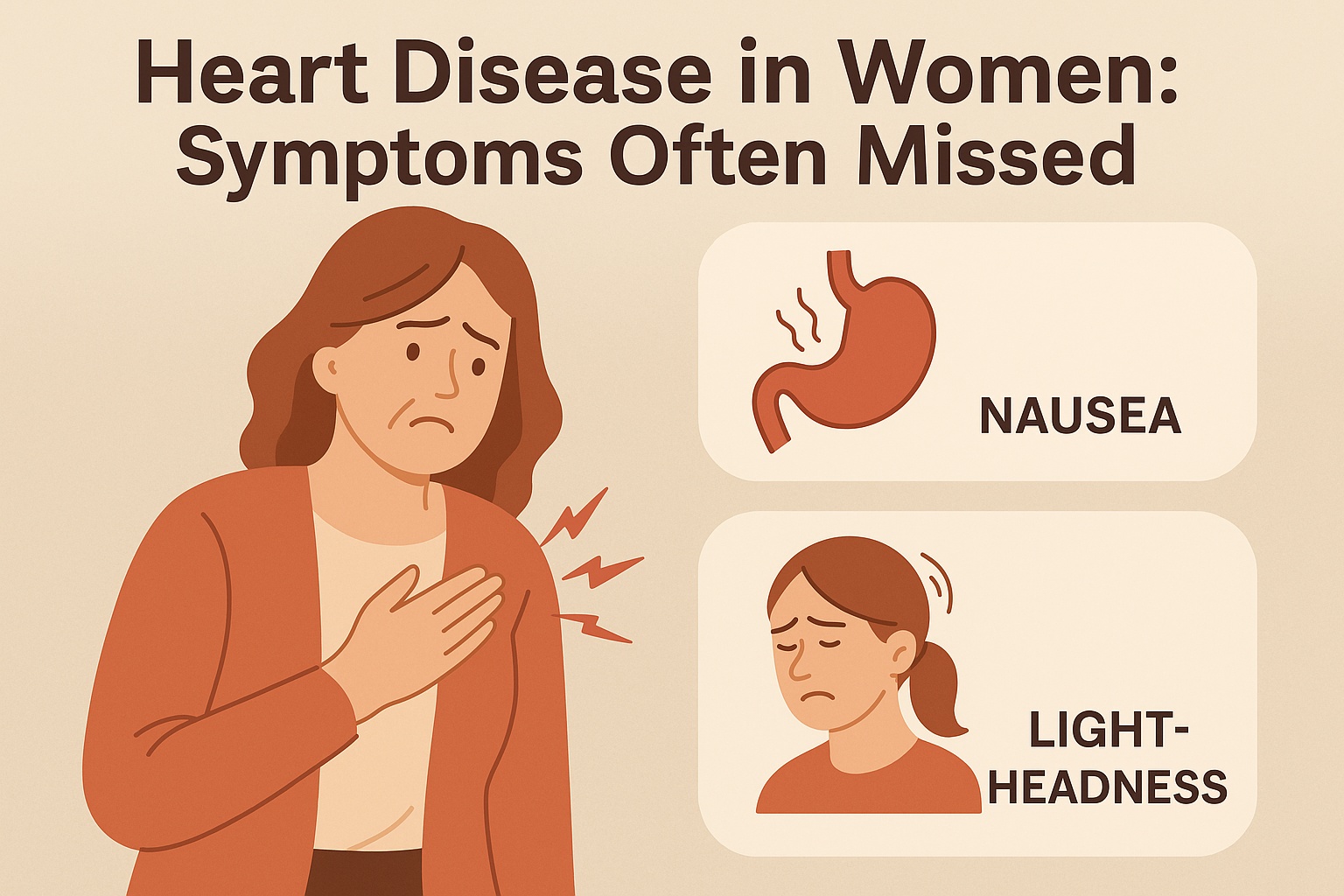
Common Symptoms of Heart Disease in Women
Recognizing warning signs can be lifesaving. Symptoms of heart disease in women may include:
- Unusual fatigue that’s persistent and unexplained
- Shortness of breath, especially during everyday activities
- Discomfort in the neck, jaw, shoulder, upper back, or abdomen
- Lightheadedness, dizziness, or fainting
- Cold sweats unrelated to physical exertion
- Nausea or vomiting
- Mild chest pain or pressure—not necessarily severe
These symptoms can occur days or even weeks before a heart attack. Women may not feel the “elephant on the chest” pressure that men often describe, making the signs easier to miss.
Risk Factors Unique to Women
While traditional risk factors like high blood pressure, high cholesterol, and smoking apply to both genders, women also face unique risks:
- Hormonal changes — Post-menopausal estrogen decline increases risk.
- Pregnancy complications — Preeclampsia, gestational diabetes, and high blood pressure during pregnancy raise lifetime heart disease risk.
- Autoimmune conditions — Disorders like lupus or rheumatoid arthritis, more common in women, heighten cardiovascular risk.
- Depression and anxiety — These mental health factors affect the heart more profoundly in women than men.
How Heart Disease Is Diagnosed in Women
If you suspect heart trouble, don’t delay testing. Diagnosis may include:
- Electrocardiogram (EKG or ECG)
- Stress tests with imaging
- Blood tests to detect cardiac enzymes or markers
- Echocardiogram or coronary angiogram
Some women may have microvascular disease (small artery blockages) that aren’t visible on standard tests. That’s why it’s crucial to work with a cardiologist who understands women’s heart health.
Effective Treatment Options for Heart Disease in Women
Heart disease in women is treatable—especially when caught early. Treatment may involve:
- Medications — Beta-blockers, statins, blood thinners, and ACE inhibitors help control symptoms and prevent complications.
- Lifestyle changes — Adopting a heart-healthy diet, increasing physical activity, quitting smoking, and reducing stress are essential.
- Surgical options — In cases of blocked arteries, angioplasty or bypass surgery may be necessary.
Prevention Tips for Women
Preventing heart disease starts with knowledge and action. Here’s how women can reduce their risk:
- Monitor blood pressure, cholesterol, and blood sugar levels regularly
- Eat a Mediterranean-style diet rich in whole grains, vegetables, fruits, and healthy fats
- Engage in at least 150 minutes of moderate-intensity exercise per week
- Limit alcohol and avoid tobacco entirely
- Prioritize sleep and mental well-being
FAQs About Heart Disease in Women
- Can heart disease in women occur without chest pain?
Yes. Many women experience symptoms like fatigue, back pain, or nausea without any chest pain. - At what age should women start screening for heart disease?
Screenings should begin in your 30s if risk factors exist, and universally by age 40–45. - Is it safe to exercise with heart disease?
In most cases, yes—but always consult your doctor before starting or changing an exercise plan.
Conclusion: Know the Signs of Heart Disease in Women
Understanding how heart disease in women presents differently can save lives. Don’t dismiss symptoms like fatigue, nausea, or shortness of breath—especially if you have risk factors. Early detection, proper testing, and personalized treatment are the keys to preventing complications. Talk to your doctor, trust your instincts, and take heart health seriously—it’s the best gift you can give yourself and those you love.